K.SWARNA MUKHI ROLL NO-198
40M WITH DECREASED URINE OUTPUT SINCE 4DAYS.
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
A 40yr old male came to the opd with -
Chief complaints -
C/o vomiting since 4days
C/o constipation since 4days
C/o decreased urine output since 4days
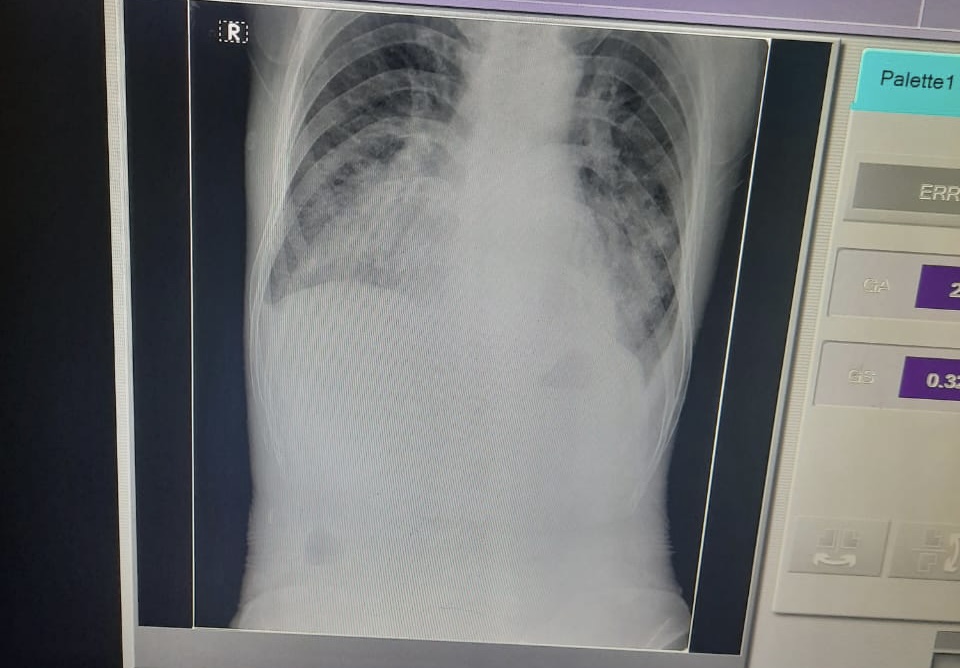
C/o shortness of breath since 4days
C/o generalized body swelling since 4days
Hopi-
Patient was apparently alright 4days back then he had vomitings since 4days ,
constipation since 4days No flatulence ,
decreased urine output since 4days .
Swelling both upper limbs and face
Sob since 4days grade-1
No orthopnea
No pnd
Past illness-
K/c/o of hypertension since 1year
Bilateral lower limb amputation was done 2years back
Personal history-
Diet -mixed
Appetite- decreased since 4days
Sleep-deprived since few days
Bowel and bladder movements-irregular
No known allergies
ADDICTION-->
Patient had the habit of drinking alcohol since teenage
Occasional beedi smoker
Patient works as a labour so he used to drink alcohol daily around 360ml whiskey ---->
FURTHER HE WOULD DRINK >760ml WHISKEY
I
1500ML WHISKEY WHEN HE DRINKS ALL DAY
Family history-not significant
General examination-
Patient is conscious , coherent , cooperative.
Vitals -
Bp-180/90mmhg
Pr-63bpm
Rr-24cpm
USG impression :
INVESTIGATIONS:
Hemogram -
Hb -10.5
Pcv-27.7
Tlc-12,500
Rbc-3.8
Plt count -1.61
INVESTIGATIONS:









Comments
Post a Comment